types of gynecological surgery in Iran
There are various types of gynecological surgery in Iran, which can be broadly categorized as non-cancerous (benign) gynecologic surgeries and gynecologic cancer surgeries in Iran. Here are some examples:
1. Non-Cancerous (Benign) Gynecologic Surgeries
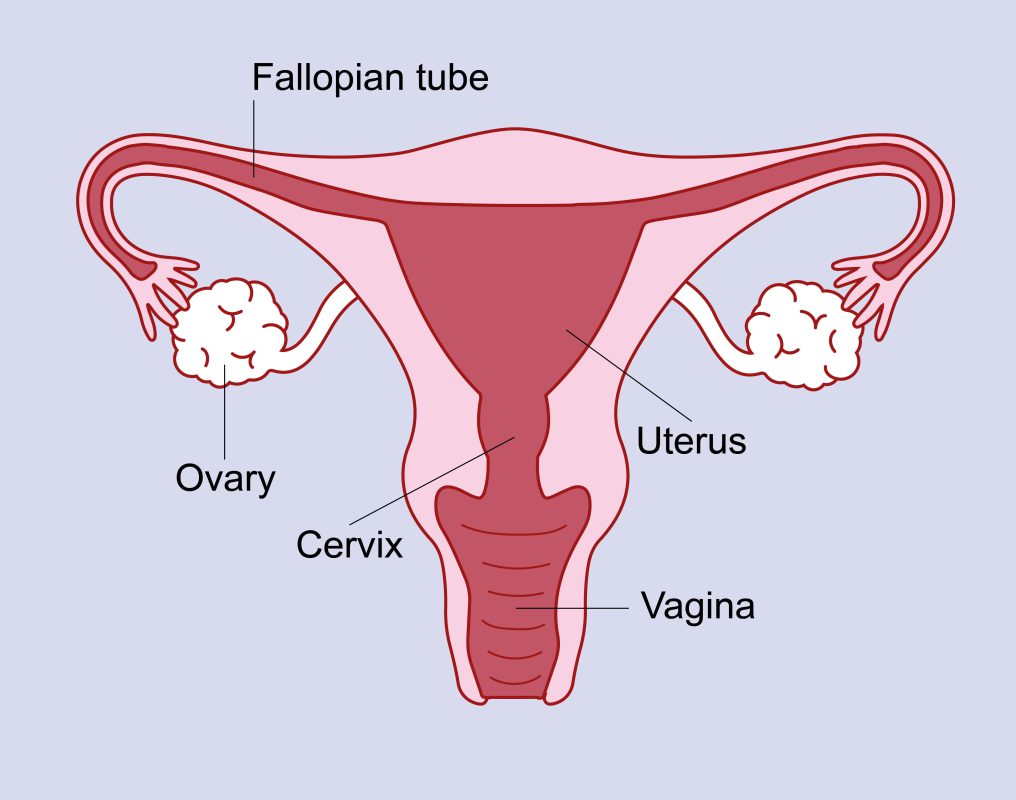
a. Hysterectomy: Surgical removal of the uterus. It can be total (removing the entire uterus and cervix) or partial (removing only the upper part of the uterus, leaving the cervix intact).
b. Oophorectomy: Surgical removal of one or both ovaries.
c. Salpingectomy: Surgical removal of one or both fallopian tubes.
d. Myomectomy: Surgical removal of uterine fibroids without removing the uterus.
e. Endometrial Ablation: Destruction of the lining of the uterus to treat heavy menstrual bleeding.
f. Laparoscopy: Minimally invasive surgery performed through small incisions. It can be used to treat conditions like endometriosis, ectopic pregnancy, pelvic inflammatory disease, and ovarian cysts.
g. Hysteroscopy: Non-invasive surgery that involves inserting a small, lighted instrument through the vagina and cervix into the uterus to diagnose or treat uterine diseases.
h. Tubal Ligation: A form of permanent birth control where the fallopian tubes are cut, tied, or otherwise blocked to prevent pregnancy.
2. Gynecologic Cancer Surgeries in Iran
a. Radical Hysterectomy: Surgical removal of the uterus, cervix, part of the vagina, and possibly nearby lymph nodes. It is often performed for cervical or endometrial cancer.
b. Pelvic Exenteration: An extensive gynecological surgery in Iran used to treat advanced pelvic cancers. It involves the removal of the bladder, uterus, lower colon, rectum, or vagina.
c. Lymph Node Dissection: Surgical removal of lymph nodes in the pelvic area to check for the spread of cancer.
d. Debulking Surgery: Surgical removal of as much of a tumor as possible. This is commonly used in the treatment of ovarian cancer.
Remember that the type and extent of gynecological surgery in Iran depend on the individual patient’s condition, overall health, and the nature and stage of the disease. Always consult with your healthcare provider to understand the best options for your specific circumstances.

Hysterectomy procedure in Iran :
A hysterectomy is a gynecological surgery in Iran that involves the removal of the uterus. It may also involve the removal of the cervix, fallopian tubes, and ovaries, depending on the specific type of hysterectomy being performed. Hysterectomy is one of the most common gynecological surgery in Iran performed on women.
Here is an overview of the different types of hysterectomy procedures:
1. Total hysterectomy: In a total hysterectomy, the entire uterus, including the cervix, is removed. The fallopian tubes and ovaries may also be removed during the procedure, which is known as a bilateral salpingo-oophorectomy.
2. Partial hysterectomy (subtotal or supracervical hysterectomy): In a partial hysterectomy, only the upper part of the uterus is removed, while the cervix is left intact. The fallopian tubes and ovaries may or may not be removed.
3. Radical hysterectomy: A radical hysterectomy is typically performed in cases of gynecological cancer, particularly cervical cancer. It involves the removal of the uterus, cervix, upper part of the vagina, and surrounding tissues. Lymph nodes in the pelvic area may also be removed.
Hysterectomy can be performed through different surgical approaches:
1. Abdominal hysterectomy: An abdominal hysterectomy is performed through an incision made in the lower abdomen. This approach allows the surgeon to have a good view of the pelvic organs and is often used for large uteri, complex conditions, or when other procedures need to be performed simultaneously.
2. Vaginal hysterectomy: During a vaginal hysterectomy, the uterus is removed through the vagina, and no external incisions are made. This approach is less invasive and generally results in a faster recovery compared to abdominal hysterectomy. However, it may not be suitable for all cases, depending on factors such as the size and condition of the uterus.
3. Laparoscopic or robotic-assisted hysterectomy: These minimally invasive approaches involve the use of specialized instruments and a small incision or multiple small incisions in the abdomen. Laparoscopic or robotic-assisted techniques offer the advantage of smaller incisions, reduced blood loss, and quicker recovery compared to traditional abdominal hysterectomy.
The choice of hysterectomy procedure depends on various factors, including the reason for the surgery, the patient’s medical history, the size and condition of the uterus, and the surgeon’s expertise. It is important to have a thorough discussion with your healthcare provider to understand the options, benefits, risks, and expected recovery associated with the specific approach recommended for your case.
Hysterectomy is considered a major surgery and carries potential risks and complications, such as bleeding, infection, injury to surrounding organs, and adverse reactions to anesthesia. Recovery time can vary but generally involves a few weeks of healing and post-operative care.
It’s essential to consult with a qualified healthcare professional to discuss your specific situation, understand the details of the procedure, and address any concerns you may have.
Oophorectomy procedure in Iran
Oophorectomy is a gynecological surgery in Iran that involves the removal of one or both ovaries. It can be performed as part of a hysterectomy (removal of the uterus) or as a standalone procedure. Oophorectomy may be recommended for various reasons, including the treatment or prevention of certain medical conditions.
Here is an overview of the oophorectomy procedure:
1. Anesthesia: Prior to the surgery, anesthesia is administered to ensure that you are comfortable and pain-free during the procedure. The type of anesthesia used (general anesthesia or regional anesthesia) will depend on factors such as your overall health and the surgeon’s preference.
2. Incisions: The surgeon will make one or more incisions in the abdominal area. The size and number of incisions may vary depending on the specific surgical technique being used, such as open surgery or minimally invasive laparoscopic surgery.
3. Ovary removal: The surgeon will carefully detach the affected ovary or ovaries from surrounding tissues and blood vessels. Special care is taken to prevent damage to nearby structures during this step.
4. Closure: After the ovaries have been removed, the surgeon will close the incisions using sutures or surgical staples. In some cases, absorbable stitches may be used, which do not require removal.
5. Recovery: Following the surgery, you will be taken to a recovery area where medical staff will monitor your vital signs. Pain medications may be administered to help manage any discomfort. The length of the hospital stay will depend on the specific circumstances of the surgery and your overall health.
Recovery time after an oophorectomy can vary depending on the surgical approach and individual factors. It’s common to experience some pain, swelling, and discomfort in the surgical area for a few days or weeks. Your healthcare provider will provide instructions on post-operative care, including wound care, pain management, and specific activity restrictions.
It’s important to note that oophorectomy can have significant implications for hormonal balance and fertility. Removal of both ovaries (bilateral oophorectomy) may induce menopause if you haven’t reached it naturally. Hormone replacement therapy (HRT) may be recommended to manage menopausal symptoms and mitigate potential long-term health effects.
If you are considering an oophorectomy, it’s crucial to discuss the procedure, its potential benefits, risks, and long-term implications with your healthcare provider. They can provide personalized guidance based on your specific medical condition, overall health, and individual circumstances.
Salpingectomy procedure in Iran
Salpingectomy is a gynecological surgery in Iran that involves the removal of one or both fallopian tubes. It can be performed for various reasons, including the treatment or prevention of certain medical conditions. Salpingectomy may be performed alone or as part of a more extensive procedure, such as a hysterectomy or oophorectomy.
Here is an overview of the salpingectomy procedure:
1. Anesthesia: Prior to the surgery, anesthesia is administered to ensure that you are comfortable and pain-free during the procedure. The type of anesthesia used (general anesthesia or regional anesthesia) will depend on factors such as your overall health and the surgeon’s preference.
2. Incisions: The surgeon will make one or more incisions in the abdominal area. The size and number of incisions may vary depending on the specific surgical technique being used, such as open surgery or minimally invasive laparoscopic surgery.
3. Fallopian tube removal: The surgeon will carefully identify and isolate the fallopian tubes. The tubes are then dissected and removed from the surrounding tissues and blood vessels. Special care is taken to prevent damage to nearby structures during this step.
4. Closure: After the fallopian tubes have been removed, the surgeon will close the incisions using sutures, surgical staples, or adhesive strips. In some cases, absorbable stitches may be used, which do not require removal.
5. Recovery: Following the surgery, you will be taken to a recovery area where medical staff will monitor your vital signs. Pain medications may be administered to help manage any discomfort. The length of the hospital stay will depend on the specific circumstances of the surgery and your overall health.
Recovery time after a salpingectomy can vary depending on the surgical approach and individual factors. It’s common to experience some pain, swelling, and discomfort in the surgical area for a few days or weeks. Your healthcare provider will provide instructions on post-operative care, including wound care, pain management, and specific activity restrictions.
Salpingectomy may be performed for various reasons, such as the treatment of ectopic pregnancy, prevention of ovarian cancer in high-risk individuals, or as a method of sterilization. It’s important to discuss the procedure, its potential benefits, risks, and long-term implications with your healthcare provider. They can provide personalized guidance based on your specific medical condition, overall health, and individual circumstances.
Myomectomy procedure in Iran
Myomectomy is a gynecological surgery in Iran performed to remove uterine fibroids, which are noncancerous growths that develop in the uterus. Unlike a hysterectomy, which involves the complete removal of the uterus, a myomectomy preserves the uterus, allowing women to potentially conceive and carry a pregnancy in the future.
Here is an overview of the myomectomy procedure:
1. Anesthesia: Before the surgery, you will be given anesthesia to ensure that you are comfortable and pain-free during the procedure. The type of anesthesia used (general anesthesia or regional anesthesia) will depend on factors such as your overall health and the surgeon’s preference.
2. Incisions: The surgeon will make one or more incisions in the abdominal area. The size and location of the incisions may vary depending on the size, number, and location of the fibroids, as well as the surgical approach chosen.
3. Fibroid removal: The surgeon will carefully locate and remove the fibroids from the uterus. The specific technique used will depend on factors such as the size and location of the fibroids. The fibroids can be removed through various methods, including:
– Abdominal myomectomy: In this approach, the surgeon makes a larger incision in the lower abdomen to access the uterus and remove the fibroids.
– Laparoscopic myomectomy: This minimally invasive approach involves making small incisions in the abdomen and using specialized instruments and a camera (laparoscope) to guide the surgeon in removing the fibroids.
– Hysteroscopic myomectomy: This technique is used when fibroids are located within the uterine cavity. A hysteroscope, which is a thin, lighted tube, is inserted through the vagina and cervix into the uterus to remove the fibroids.
4. Closure: After the fibroids have been removed, the surgeon will close the incisions using sutures, surgical staples, or adhesive strips. In some cases, absorbable stitches may be used, which do not require removal.
5. Recovery: After the surgery, you will be taken to a recovery area where medical staff will monitor your vital signs. You may experience pain, swelling, and discomfort in the surgical area for a few days or weeks. Pain medications may be prescribed to help manage your discomfort. The length of the hospital stay will depend on the specific circumstances of the surgery and your overall health.
Recovery time after a myomectomy varies depending on the surgical approach, the size and number of fibroids removed, and individual factors. Your healthcare provider will provide instructions on post-operative care, including wound care, pain management, activity restrictions, and when it is safe to resume normal activities.
It’s important to note that myomectomy is intended for women who wish to preserve their fertility or retain their uterus. However, there is a risk of fibroid recurrence, as new fibroids can develop in the future. It’s crucial to discuss the procedure, its potential benefits, risks, and long-term implications with your healthcare provider. They can provide personalized guidance based on your specific medical condition, overall health, and reproductive goals.
Endometrial Ablation procedure in Iran
Endometrial ablation is a gynecological surgery in Iran used to treat abnormal uterine bleeding by removing or destroying the lining of the uterus (endometrium). It is typically performed as a minimally invasive procedure and is an alternative to a hysterectomy for women who do not wish to or cannot undergo a more extensive surgery.
Here is an overview of the endometrial ablation procedure:
1. Anesthesia: Before the procedure, anesthesia is administered to ensure your comfort. The type of anesthesia used can vary and may include local anesthesia, regional anesthesia, or general anesthesia, depending on the specific technique and your preferences.
2. Preparation: Your healthcare provider will clean the cervix and vagina with an antiseptic solution. In some cases, medications may be given to help dilate the cervix, making it easier to access the uterus.
3. Access to the uterus: The surgeon will insert a thin instrument called a hysteroscope through the cervix and into the uterus. The hysteroscope allows the surgeon to visualize the uterine cavity and guide the procedure.
4. Removal or destruction of the endometrium: The specific technique used for endometrial ablation can vary. Common methods include:
– Thermal ablation: Heat energy, such as radiofrequency energy, heated fluid, or laser energy, is used to destroy the endometrial tissue.
– Cryoablation: Extreme cold is used to freeze and destroy the endometrium.
– Microwave ablation: Microwaves are used to heat and destroy the endometrial tissue.
– Balloon ablation: A balloon device is inserted into the uterus and filled with heated fluid, which destroys the endometrial tissue.
– Radiofrequency ablation: Radiofrequency energy is applied to the endometrium to destroy it.
5. Monitoring and completion: Throughout the procedure, the surgeon will monitor the progress and ensure that the appropriate areas of the endometrium are treated. Once the desired extent of ablation is achieved, the instruments are removed.
6. Recovery: After the procedure, you will be taken to a recovery area to be monitored. You may experience cramping, mild pain, or vaginal discharge following the procedure. Pain medications or anti-inflammatory drugs may be prescribed to manage any discomfort. Recovery time is generally shorter than with more invasive procedures like a hysterectomy.
It’s important to note that endometrial ablation is not suitable for everyone. It is typically recommended for women who have completed childbearing or do not wish to have more children, as it can affect fertility. Additionally, it may not be appropriate for women with certain medical conditions or those with large uterine fibroids.
Discussing the procedure, its potential benefits, risks, and long-term implications with your healthcare provider is crucial. They can provide personalized guidance based on your specific medical condition, overall health, and individual circumstances to determine if endometrial ablation is a suitable option for you.
Pelvic Exenteration procedure in Iran
Pelvic exenteration is a complex gynecological surgery in Iran performed in cases of advanced pelvic cancers that have spread to nearby organs and tissues. It involves the removal of multiple organs within the pelvic cavity, which may include the uterus, cervix, vagina, ovaries, fallopian tubes, bladder, rectum, and part of the colon.
Here is an overview of the pelvic exenteration procedure:
1. Preoperative evaluation: Before the surgery, a thorough evaluation is conducted to determine the extent of the cancer and its involvement with nearby structures. Imaging studies, such as CT scans or MRI, are often used to assess the tumor’s size, location, and spread.
2. Anesthesia: Prior to the surgery, anesthesia is administered to ensure that you are asleep and pain-free during the procedure. The specific type of anesthesia used will be determined by the surgeon and anesthesiologist based on your overall health and the anticipated duration of the surgery.
3. Incisions: The surgeon will make a large abdominal incision to access the pelvic cavity. The size and location of the incision will depend on the specific case and the surgeon’s preferred approach.
4. Organ removal: The surgeon will carefully dissect and remove the affected organs, which may include the uterus, cervix, vagina, ovaries, fallopian tubes, bladder, rectum, and part of the colon. The goal is to remove all visible tumor tissue while preserving as much healthy tissue as possible.
5. Reconstruction: After the necessary organs have been removed, the surgeon will proceed with reconstructive procedures to restore some functions and preserve quality of life. This may involve creating a new urinary diversion (such as an ileal conduit or neobladder) to redirect urine flow, creating a colostomy or ileostomy for bowel elimination, and reconstructing the vaginal canal (if feasible).
6. Closure: Once the organs have been removed and reconstructed, the surgeon will close the incisions using sutures or staples. Drainage tubes may be placed to remove excess fluid or blood from the surgical site.
7. Recovery: Following the surgery, you will be closely monitored in the intensive care unit (ICU) or a specialized postoperative unit. The recovery process can be lengthy and may involve pain management, monitoring of vital signs, wound care, and physical therapy. The hospital stay can range from several days to a few weeks, depending on individual factors and the extent of the surgery.
Pelvic exenteration is a major surgery with significant risks and potential complications, including infection, bleeding, leakage from reconstructed organs, blood clots, and damage to surrounding structures. It is generally reserved for cases where the cancer has spread extensively and other treatment options have been exhausted.
It’s important to have a thorough discussion with your healthcare team to understand the potential benefits, risks, and long-term implications of pelvic exenteration. They will provide you with personalized guidance based on your specific cancer diagnosis, overall health, and individual circumstances.
Lymph Node Dissection procedure in Iran
Lymph node dissection, also known as lymphadenectomy, is a gynecological surgery in Iran performed to remove lymph nodes in a specific area of the body. It is commonly done as part of the staging and treatment for certain types of cancer, particularly cancers that are likely to spread to the lymph nodes.
Here is an overview of the lymph node dissection procedure:
1. Anesthesia: Before the surgery, anesthesia is administered to ensure your comfort during the procedure. The type of anesthesia used can vary and may include general anesthesia or regional anesthesia, depending on the extent and location of the lymph node dissection.
2. Incision: The surgeon will make an incision in the area where the lymph nodes are located. The size and location of the incision will depend on the specific area being treated. For example, in breast cancer, the incision may be made in the armpit or along the breast area.
3. Identification and removal of lymph nodes: The surgeon will carefully identify and dissect the lymph nodes in the area. The number of lymph nodes removed can vary depending on the specific case and surgical goals. The surrounding tissues and blood vessels are carefully preserved during the dissection.
4. Biopsy and examination: The removed lymph nodes are sent to a pathology laboratory for examination. The pathologist will analyze the lymph nodes to determine if cancer cells are present. This information helps in staging the cancer and determining the appropriate treatment plan.
5. Closure: After the lymph nodes have been removed, the surgeon will close the incision using sutures or surgical staples. In some cases, drainage tubes may be placed to remove excess fluid from the surgical site.
6. Recovery: Following the surgery, you will be taken to a recovery area where medical staff will monitor your vital signs. Pain medications may be prescribed to manage any discomfort. The length of the hospital stay will depend on the specific circumstances of the surgery and your overall health.
Lymph node dissection carries potential risks and complications, which can include infection, bleeding, lymphedema (swelling due to impaired lymphatic drainage), numbness or tingling in the surgical area, and limited range of motion. These risks will be discussed with you by your healthcare team before the surgery.
Lymph node dissection is often performed in conjunction with other cancer treatments, such as surgery to remove the primary tumor or radiation therapy. The specific approach and extent of lymph node dissection will depend on the type and stage of cancer, as well as individual factors.
It’s important to have a detailed discussion with your healthcare provider to understand the specific goals, risks, and potential benefits of lymph node dissection in your case. They will provide personalized guidance based on your specific medical condition, overall health, and individual circumstances.
Debulking Surgery procedure in Iran
Debulking surgery, also known as cytoreductive surgery, is a gynecological surgery in Iran performed to remove as much visible tumor mass as possible in cases of advanced cancer. The goal of debulking surgery is to reduce the tumor burden and improve the effectiveness of subsequent treatments, such as chemotherapy or radiation therapy.
Here is an overview of the debulking surgery procedure:
1. Anesthesia: Before the surgery, anesthesia is administered to ensure your comfort during the procedure. The type of anesthesia used will depend on the extent and location of the surgery. It may be general anesthesia, which puts you to sleep, or regional anesthesia, which numbs the specific area being operated on.
2. Incision: The surgeon will make an incision in the area where the tumor is located. The size and location of the incision will depend on the specific type of cancer and its location in the body.
3. Tumor removal: The surgeon will carefully dissect and remove as much visible tumor mass as possible. This may involve removing the primary tumor and any metastatic tumors present in nearby organs or tissues. In some cases, adjacent structures may also be removed if they are involved with the tumor.
4. Reconstruction: After the tumor has been removed, the surgeon may perform reconstructive procedures to restore or maintain organ function, if necessary. This may involve reconnecting or rerouting blood vessels, restoring continuity of the digestive tract, or reconstructing other affected structures.
5. Closure: Once the tumor has been removed and any necessary reconstruction is completed, the surgeon will close the incision using sutures or surgical staples. Drainage tubes may be placed to remove excess fluid or blood from the surgical site.
6. Recovery: Following the surgery, you will be taken to a recovery area where medical staff will monitor your vital signs. Pain medications will be provided to manage any discomfort. The length of the hospital stay will depend on the specific circumstances of the surgery and your overall health.
Debulking surgery can be a major procedure with potential risks and complications, including infection, bleeding, damage to surrounding structures, and impaired organ function. These risks will be discussed with you by your healthcare team before the surgery.
Debulking surgery is often performed as part of a multidisciplinary approach to cancer treatment. It is typically followed by additional therapies, such as chemotherapy or radiation therapy, to target any remaining cancer cells that may not have been completely removed during surgery.
It’s important to have a detailed discussion with your healthcare provider to understand the specific goals, risks, and potential benefits of debulking surgery in your case. They will provide personalized guidance based on your specific cancer diagnosis, overall health, and individual circumstances.